RICHMOND, Va. — Members of Virginia's newly created nursing home advisory board, which was established in an effort to improve quality and accountability in the long-term care system, engaged in at-times passionate and emotional discussion during its second meeting in Richmond on Thursday.
During the meeting, board member Sam Kukich delivered a blunt message to the body: “We have a fire. We have a bad fire. The house is burning down."
Kukich founded her advocacy organization Dignity for the Aged after she said her mother-in-law received inadequate care at five different facilities in the Tidewater region between 2016 and 2019.
"I had no idea that when we were paying $10,000 a month that there would be any issues with regard to basic hygiene, feeding, theft, abuse and neglect. Little did I know that the regulations and laws would be ignored and my mother-in-law would be subjected to life without proper care or dignity," she said.
When her mother eventually died in a nursing home at 1:00 in the morning, Kukich said she pushed the call light to alert staff of the death, but she "couldn't find anyone to tell.” Since then, she's been on a mission to educate other families and push for reform.
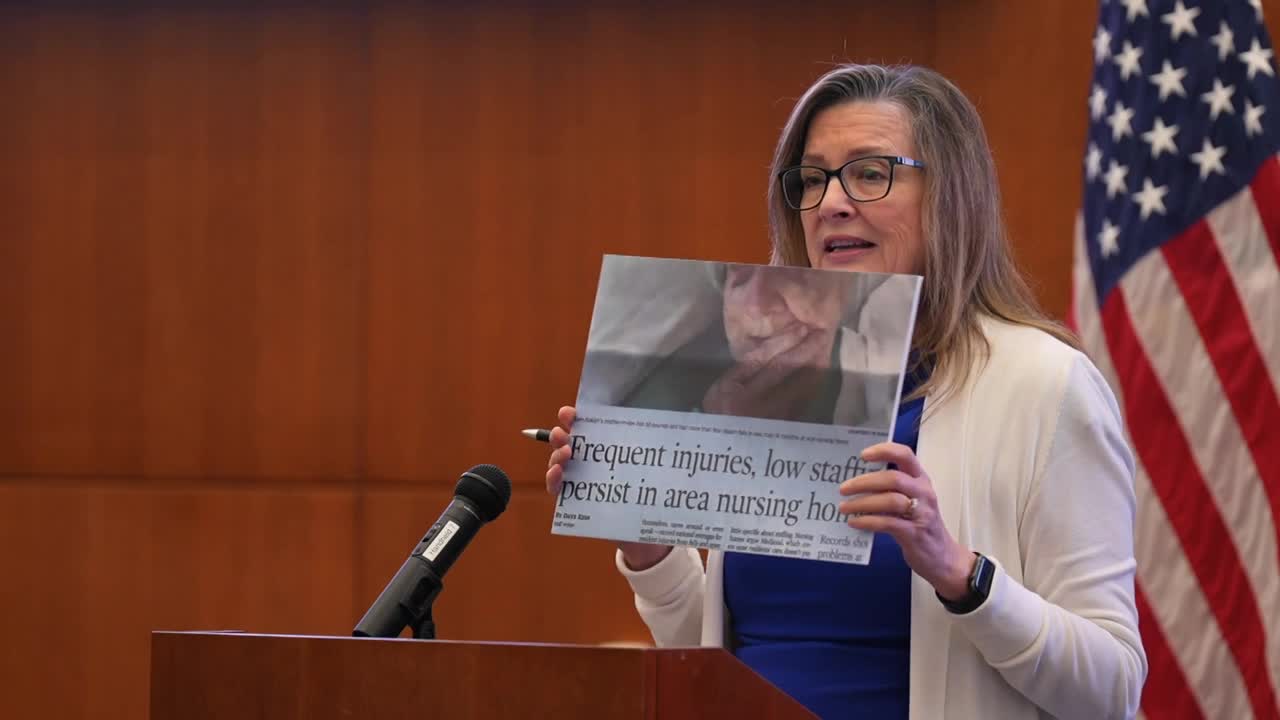
On Thursday, Kukich presented research to her fellow board members showing 141 of Virginia's nursing homes, nearly half of all facilities statewide, are on an abuse watch list. That's according to an advocacy organization that tracks staffing levels, quality ratings, and inspection results.
The underlying issues to low staffing levels and poor quality ratings, she believes, include:
1.) Minimal tracking of how facility owners spend money, much of which are Medicare and Medicaid dollars, especially through related-party transactions.
“There appears to be little to no scrutiny by the federal government on how this money is spent. Private equity corporations are buying up nursing homes for profit, and no one understands the web of hidden ownership," she said.
And 2.) Lacking enforcement of residents' rights.
“Right now they are in warehouses waiting to die," Kukich said.
Another resident advocate on the board, Joanna Heiskill, agreed and said many family members with loved ones in facilities feel they "go in there and die."
But nursing home administrator Todd Barnes of the Department of Veterans Services, who runs a government-operated facility with high quality ratings, warned the board against casting all providers in a negative light.
“I think there needs to be that increased oversight and guidance to those nursing homes that need help to be efficient. But I think it's important that you bring in all the players, and you recognize that there are a lot of buildings that are giving exceptional care," Barnes said.
That sentiment was echoed by Jonathan Cook, the CEO of a chain of not-for-profit faith-based facilities.
"The vast majority of the individuals who go to work, whether it's a [nurse aide] or a housekeeper, a nurse or administrator, they are caring, compassionate people who want to serve human beings. Now are there some players out there that are motivated by profit? Yes," Cook said.
One of those compassionate caregivers is board member Candace Gilliam, a licensed practical nurse for August Healthcare.
“I love being a nurse. I love taking care of my residents," Gilliam told CBS 6.
But she said she simply doesn't have enough help to do her job, especially after the pandemic wreaked havoc on the industry.
On any given day, she's assigned to care for 15 residents while nurse aides, who typically handle tasks such as feeding and bathing, have a resident ratio of one aide to ten residents.
“Some people may not understand if I have two feeders in my set, and it did take me 45 minutes to feed this one person— that other one, they don't understand. Their loved one comes in, and they want to know, why wasn't that person fed? Why did it take 45 minutes for somebody to get back there? I don't have anybody else. It's just me," she said. "Having a large nurse to patient ratio, it changes the care that you provide. Sometimes you do feel like you could have done more today, but you just didn't have the time."
Gilliam believes many abuse and neglect cases in facilities are not intentional but rather a symptom of a strained workforce.
"When we speak about the Virginia Department of Health and the struggles that they're in right now with being in such a delay with surveys (inspections), it was because of staffing, and we got this board together to enforce their staffing. But what are we doing in nursing homes to push our staffing? Because we need it," Gilliam said.
As the board works to identify and address root problems, family members like Janet Payne say they're suffering. Payne attended Thursday's meeting to give public comment.
“I lived a nightmare with my mother. She had 30 falls in a nursing home, three falls in the last two days of her life — that killed her," Payne said.
Payne said her mother died in a Hanover facility last Halloween.
She said she filed a complaint with the Virginia Department of Health (VDH) and that it took the agency a year to investigate. She said VDH eventually substantiated her complaint but found no deficiencies.
"I called and called and called attempting to get an explanation. Nobody is calling back," she said.
The understaffed VDH office responsible for overseeing nursing homes has been criticized by some family members over the past year for being unresponsive to their complaints. Those concerns were highlighted in previous CBS 6 investigations, showing Virginia ranked almost last in the country for completing timely inspections of facilities as regulators observed declining quality of care.
On Thursday, agency officials informed the board about its efforts to aggressively fill vacancies, as directed by an executive order issued by Governor Youngkin in August. They said more than 1,000 people have applied for open positions in the office since July 2025, and 14 facility inspectors have since accepted offers. New leaders are also expected to join the office in mid-November.
Toward the end of the meeting, board members were asked to sign up for one of three different subgroups to start discussing solutions and policy recommendations. Those focus areas include ownership transparency, financial reporting, vetting and licensing, the inspection process, and family engagement.
The board is expected to meet again in mid-November and go over those ideas. The goal is for the board to present final recommendations to the administration and state health commissioner by the end of the year.
CBS 6 is committed to sharing community voices on this important topic. Email your thoughts to the CBS 6 Newsroom.
📲: CONNECT WITH US
Blue Sky | Facebook | Instagram | X | Threads | TikTok | YouTube